Related Research
Learn more about our studies
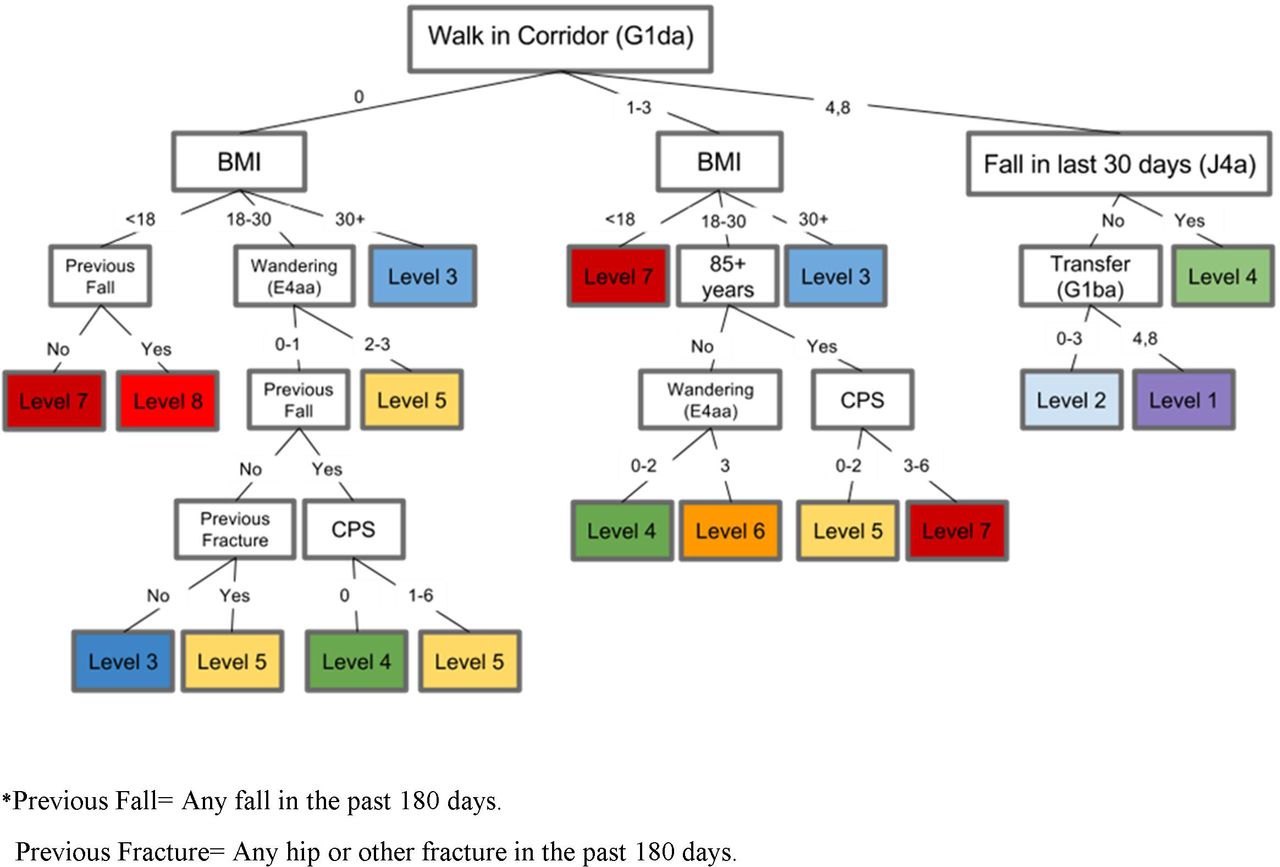
Overview: The Geras Centre for Aging and Research led the development of an evidence-based fracture risk scale (FRS) that predicts hip fracture over a 1-year duration. The FRS includes LTC-specific risk factors for hip fracture and does not require bone mineral density measurements. The FRS is a standardized instrument that automatically generates fracture risk assessments for residents as part of the Resident Assessment Instrument Minimum Data Set Version 2.0 (RAI-MDS 2.0).

| Study Type: | Retrospective Cohort Study |
| Participants (N): | 29 848 LTC (Long-Term Care) Residents |
| Primary Purpose: | Development and Validation |
| Methods: |
All admission assessments completed in Ontario LTC homes from 1 April 2006 to 31 March 2010 (n=47556) were selected. Those with multiple admissions were excluded (n=4041). Among the unique admissions (n=43515) those reported on the RAI-MDS 2.0 to have end-stage disease (n=511), were comatose (n=12), received hospice (n=16) or respite care (n=785), expected a short stay (n=4016) or admission assessment completed more than 14days after the date of admission (n=4105) were excluded. Those who had no reassessments during the 1-year follow-up (n=4222) were also excluded. |
| Results: | A total of 29 848 LTC residents were enrolled in the study. Of these 22 386 were included in the derivation dataset and 7462 individual were included in the validation dataset. Approximately 2/3 of the entire sample were women and 45% were 85 years of age or older. A total of 1553 (5.2%) fractures were reported over the 1-year time period. Of these, 959 (61.8%) were hip fractures. Following a hip fracture, 6.3% of individuals died in the emergency department or as an inpatient admission and did not return to their LTC home. Using decision tree analysis, our final outcome scale had eight risk levels of differentiation. The percentage of individuals with a hip fracture ranged from 0.6% (lowest risk level) to 12.6% (highest risk level). The area under the curve of the outcome scale was similar for the derivation (0.67) and validation (0.69) samples, and the scale exhibited a good level of consistency. |
| Conclusion: | Our FRS predicts hip fracture over a 1-year time period and should be used as an aid to support clinical decisions in the care planning of LTC residents. Future research should focus on the transformation of our scale to a Clinical Assessment Protocol and to assess the FRS in other healthcare settings. |
High-Impact Research